How Risk-Bearing Entities Work Together to Succeed at Population Health
Integrating healthcare delivery between risk-bearing entities, such as providers and insurers, is, on the surface, an important step towards population health management and value-based goals. However, even vertically integrated units tend to function separately around patient care. As a result, patients are spread thin between receiving care, navigating insurance, and more—a situation that degrades the patient experience, thwarts optimal outcomes, and interferes with value-based goals. However, some organizations are bridging the gap between healthcare entities to improve quality and decrease costs of caring for at-risk patient populations through a sustainable, collaborative population health model. By joining forces and using analytics to drive decisions and scale programs, truly integrated risk-bearing entities put patients at the center of care, meeting their healthcare needs in a more efficient, cost-effective way.
Jump to:
Downloads
Health systems and other risk-bearing entities (e.g., insurers) tend to function separately around patient care, even when these units vertically integrate. For example, a patient must often have phone calls and meetings about insurance coverage in addition to already time-intensive medical appointments—a lack of collaboration that thwarts optimal patient experience, outcomes improvement, and progress towards value-based care (VBC).
Some forward-thinking healthcare organizations have realized hidden opportunities in bridging this separation between healthcare entities to improve quality and decrease costs of caring for at-risk patient populations. The path to better care and lower cost often lies in breaking down the barriers between elements, enabling a systemwide structure to manage a sustainable population health care model that improves the quality and reduces costs associated with a fully at-risk (capitated) population.
A Successful Population Health Care Model: Integration Puts Patients at the Center of Care Delivery
Despite the promise of more integrated care delivery, some healthcare leaders find that further engaging at-risk patients around insurance coverage is more difficult than it sounds, as care often revolves around the care delivery process—not the patient. For example, an individual undergoing acute care, such as cancer treatment, is likely reluctant to have conversations around billing and coverage in addition to their many medical appointments.
As an alternative to more time burdens on patients, some organizations take a patient-centered approach, bringing the insurance conversation and other care management services to patients within the flow of care. In such population-based models, as seen as between Carle Health and health plan Health Alliance, interdisciplinary care management teams meet individuals at their providers’ offices or virtually during appointment times to blend care delivery and insurance services (e.g., case management and utilization management).
Entities use data and analytics to identify populations for which a population health care delivery model will have the greatest impact. Organizations that successfully integrate a comprehensive care experience can see positive ROI and meaningful reductions in emergency department (ED) admissions and facility readmissions.
How Does an Integrated Model Manages Multiple Populations and Support Value-Based Care?
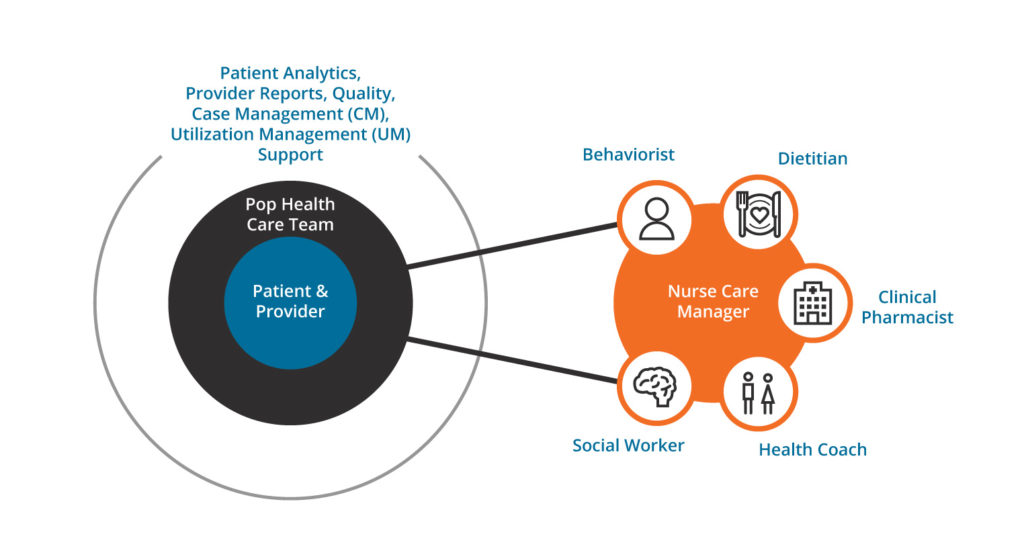
Value-based payment models vary but generally follow similar structures and key performance indicators (KPIs). These KPIs include quality performance, utilization, and medical-loss ratio. As a result, integration into a single population health delivery model aligns overall activity to larger populations and focuses efforts to drive cost and quality, removing silos and creating a best-in-class care delivery model (Figure 1).

Following the above integration map, implementing a successful population health care model within a provider practice requires the right staffing and model design. This structure includes the following:
- Multidisciplinary work groups to design the new care model for staffing and operations.
- Process mapping to develop process workflows for each position in the new model.
- Risk scoring and analytics to implement a new composite risk score to generate actionable insights and power identification and stratification.
- Provider engagement to engage clinical staff with leadership champions and population health education sessions.
- Project management to deploy standard processes to communicate progress and manage performance.
- Communication and change management to deploy proactive change management strategies to share timely information.
The Care Place of Delivery: Approach and Methodology
To support their population health care model, Carle Health and Health Alliance conceived the care place of delivery (POD) approach. PODs are embedded sites that utilize care managers and teams at a primary care provider’s (PCP) location. Additionally, virtual PODs leverage clinicians similarly, but do so virtually (e.g., phone calls, online interactions, etc.)
The POD approach capitalizes on naturally occurring care patterns (e.g., PCP visits) with specialty providers serving the same patient population. A clustering software algorithm uses claims data to identify optimal POD settings, and analysts use population density and PCP/specialty patterns to allocate embedded and virtual support for selected POD sites.
The clustering algorithm uses data, including interactions between patients and providers throughout the year to identify providers with the most interactions in common. For example, Carle Health and Health Alliance identified five locations for PODs and evaluated resources across the systems to support their population heath care model. The organizations only needed to add three roles to enable the care model—one pharmacist and two patient access coordinators. The resulting model integrates the care experience with the patient at its center (Figure 2).
The Population Health Care Model Operating Model
The population health care operating model combines care team PODs and a care model resource center to achieve the following benefits:
Integrated Care Team PODs
The care team PODs enable better care management via embedded and virtual resources. They also promote more collaboration among clinical care teams and generate a comprehensive view of care across the continuum.
Administrative Support
The population health care model allows administrative support to focus on less complex care management needs, arrange support to address social determinants of health, and conduct patient engagement outreach (e.g., post-discharge follow-up calls).
Technical and Digital Enablers
Technical and digital enablers support virtual visits, use standardized toolkits to enable efficient and effective workflows, automate manual tasks to improve resource efficiency, and analyze data to support proactive patient outreach.
In-person and virtual resources work with the population to identify patients at high-risk. After patients follow-up with their PCPs, the health systems assign the patients care managers, who connect the patients with necessary resources. The patient then consults with the appropriate specialists (e.g., cardiologists and endocrinologists), with efforts to combine appointments to limit travel requirements and conduct other visits virtually. Finally, the patient follows up virtually with her PCP and care manager to assess progress.
Measuring Success in a Population Health Care Model
Organizations can initially measure population health care model effectiveness by tracking KPIs, including sustained participation rate, predicted future costs, per member per month, participant and provider experience, and gaps in care (e.g., hypertension control). As the model matures, systems can look at financial ROI benefit-to-cost ratio, utilization reduction, and quality improvement.
In case of Carle Health and Health Alliance, patients described positive experiences, and KPIs indicated positive outcomes. For example, after factoring in COVID-19 impacts on care delivery, ED utilization rates were down 30 to 45 percent between January and December 2020, and readmission rates decreased by almost 30 percent. Per member per month decreased by 19 percent, and the model’s cost-benefit ratio (ROI and cost avoidance) was 3.1:1. Meanwhile, data showed no reduction in quality of care under the population model.
Integrating for Better Care, Lower Costs
As Carle Health and Health Alliance have demonstrated, integration across risk-bearing entities is an effective strategy towards improved care delivery and value-based goals. By joining forces and using analytics to drive decisions and scale programs, these organizations have put patients at the center of care, ensuring their needs are met at the right time and place, with minimal burden.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
- Deliver Better Population Health by Avoiding Three Mistakes
- Four Population Health Management Strategies that Help Organizations Improve Outcomes
- Population Health Management: A Path to Value
- Understanding Population Health Management: A Diabetes Example
- Value-Based Care: Four Key Competencies for Success
PowerPoint Slides
Would you like to use or share these concepts? Download presentation highlighting the key main points.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.
