Machine Learning, Predictive Analytics, and Process Redesign Reduces Readmission Rates by 50 Percent

- 39 percent relative reduction in all-cause 30-day readmissions.
- 52 percent relative reduction in 30-day readmission of patients with a principle diagnosis of heart failure.
The estimated annual cost of readmissions for Medicare is $26 billion, with $17 billion considered avoidable. Readmissions are driven largely by poor discharge procedures and inadequate followup care. Nearly one in every five Medicare patients discharged from the hospital is readmitted within 30 days.
The University of Kansas Health System had previously made improvements to reduce its readmission rate. The most recent readmission trend, however, did not reflect any additional improvement, and failed to meet hospital targets and expectations.
To further reduce the rate of avoidable readmission, The University of Kansas Health System launched a plan based on machine learning, predictive analytics, and lean care redesign. The organization used its analytics platform, to carry out its objectives.
The University of Kansas Health System substantially reduced its 30-day readmission rate by accurately identifying patients at highest risk of readmission and guiding clinical intervention.:
REDUCING READMISSIONS IS A QUALITY AND COST IMPERATIVE
Readmissions are expensive and consume a disproportionate share of expenditures for inpatient hospital care. In 2011, an estimated 3.3 million adults in the U.S. were readmitted to the hospital within 30-days of discharge, resulting in approximately $41.3 billion in hospital costs.1 For health systems seeking to improve their bottom line, reducing readmissions can significantly reduce organizational cost.
The estimated annual cost of readmissions for Medicare is $26 billion, with $17 billion considered avoidable. Readmissions are driven largely by poor discharge procedures and inadequate followup care. Nearly one in every five Medicare patients discharged from the hospital is readmitted within 30 days.2
Building on a legacy of patient care that began in 1906, The University of Kansas Health System in Kansas City, a leader in medical research and education, is a world-class academic medical center and destination for complex care and diagnosis. The University of Kansas Physicians, the largest multispecialty group practice in Kansas, comprises researchers and educators expanding the boundaries of medical knowledge.
HOSPITAL READMISSION RATE IS AN ESSENTIAL METRIC IN QUALITY IMPROVEMENT
Understanding that hospital readmission rates are an important indicator of quality of care, The University of Kansas Health System had invested in improvement efforts and successfully reduced its readmission rate. The most recent readmission trend, however, wasn’t showing the additional improvement that was anticipated, and failed to meet hospital targets.
Using lean methodology as its performance improvement framework, The University of Kansas Health System determined that a lack of standard work for discharge, and limited interdisciplinary transparency across the system resulted in high variability across inpatient units and care providers. The organization also had limited insight into a patient’s risk for readmission prior to the patient’s discharge, decreasing the ability to provide interventions to prevent readmission. A review of the 30-day readmission data showed two common reasons for readmission: an inadequate plan of care at discharge and advancement of chronic disease.
Upon analysis of available data, The University of Kansas Health System determined patients who were diagnosed with high-risk chronic disease and had more than one 30-day readmission had the greatest impact on 30-day readmission rates. However, to effectively prevent avoidable, costly readmission, the health system needed the ability to predict which patients were high risk, and needed to implement standard work and interventions to prevent readmission.
THREE CRITICAL WORK AREAS IN REDUCING READMISSION
To further reduce the rate of avoidable readmission, The University of Kansas Health System developed a plan focused on three major areas:
1. Educating and engaging health system leaders to facilitate clinical improvement
The University of Kansas Health System prepares and engages leaders in the organization to manage lean improvement work to systematically spread and manage standard work across multiple work groups. It provides lean education at a variety of levels, including introductory courses for lean process improvement and lean leadership concepts, training for all health system employees, hands-on development for front line leaders, and a more intensive, six-month program, providing hands-on learning, improving the effectiveness of its clinical improvement efforts.
2. Using machine learning to avoid costly readmissions
The University of Kansas Health System identified that it needed to better understand its patients’ risk for readmission. It was believed that if additional factors were identified and built into a model for predicting risk for readmission that was highly accurate, the organization would have the ability to identify those patients most likely to be readmitted and why, would enable caregivers to deliver focused interventions to vulnerable patients, preventing 30-day readmissions, and maximizing the effectiveness of limited resources.
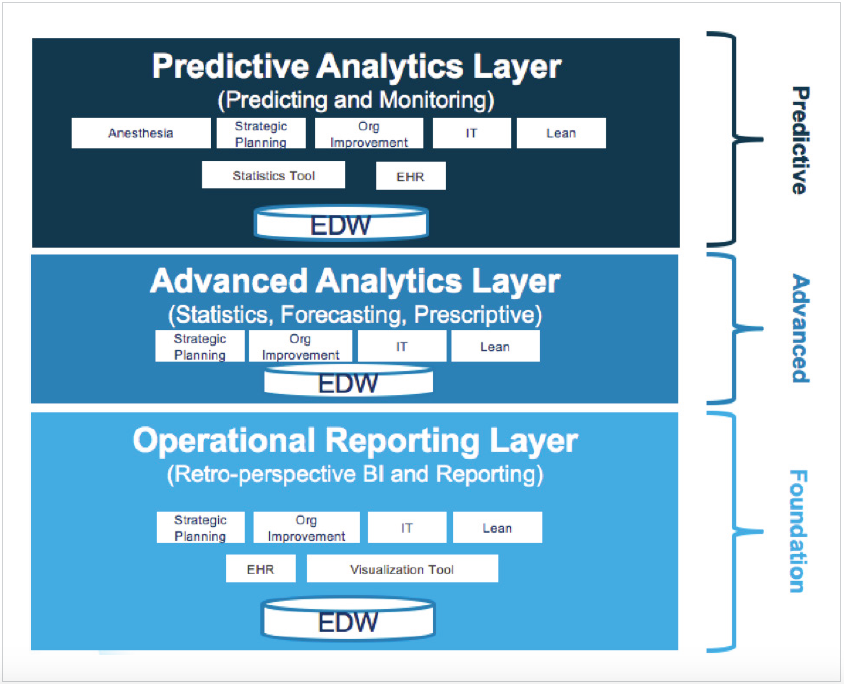
The organization used the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications as its infrastructure and primary source for data and analytics (see Figure 1). The data warehouse enabled the organization to automate extraction, aggregation, and integration of clinical, financial, administrative, patient experience, and other relevant data, as well as to apply advanced analytics to organize and measure clinical, patient safety, cost, and patient outcomes.
By applying machine learning against this rich data warehouse, risk factors could be identified that were previously unrecognized, and previously identified risk factors that were not really predictive, could be excluded. Leveraging the analytics platform to develop an advanced application to perform multi-variant risk analysis, The University of Kansas Health System identified key risk factors for readmission. It engaged dedicated business and clinical subject matter experts to drive the analytic work and develop a predictive model to provide insight into high-risk patients.
The predictive model uses variables including the Medicare severity diagnosis related group (MS-DRG), use of tobacco, residential zip code, financial risk, healthcare utilization, age, marital status, admission source, medication, provider, and more. Using machine learning, predictive analytics, and data mining techniques, The University of Kansas Health System gained new insights about their patient populations (see Figure 2).
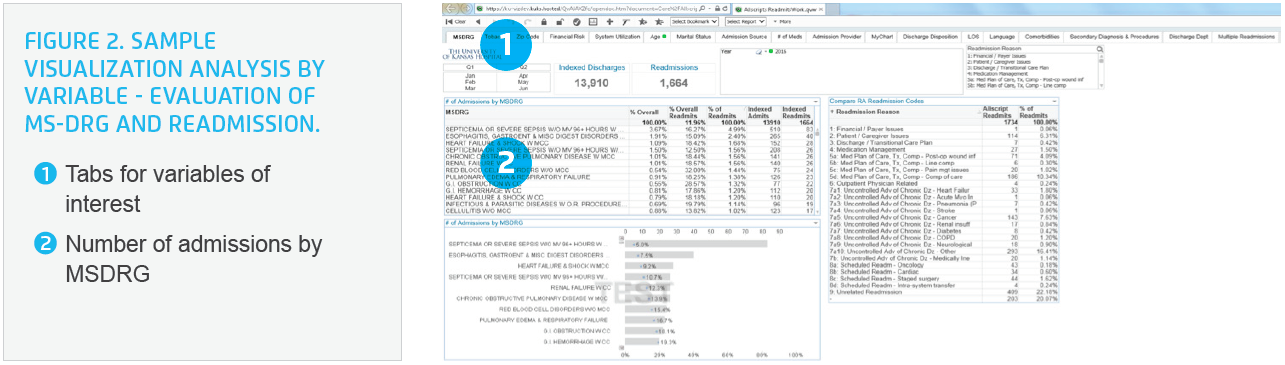
Initially, the team thought patients on a larger number of medications would be at greatest risk for readmission. The data revealed, however, that patients with no medications were at the greatest risk. Data showed similar patterns regarding age: though people often assume older patients are at the highest risk, the organization’s data show that its younger patients were at greatest risk. Of comorbidities, patients with acute kidney failure were at the highest risk for readmission.
By leveraging more than 30 published readmission models, The University of Kansas Health System developed its custom algorithm for machine learning processes to identify patterns and mathematically optimize the algorithm. Using machine learning and predictive analytics, the health system extracted information from existing datasets to identify patterns and predict outcomes and trends.
3. Providing the infrastructure to reduce variation in discharge planning and care transitions
The health system established a continuum of care strategic plan to help guide the development and infrastructure required to successfully transition the patient through all care settings in a consistent way. Initially focusing on patients with a diagnosis of heart failure, it identified the need for outreach beyond the acute care setting to make lasting reductions in the 30-day readmission rates.
To support the execution of this strategic plan, executive sponsors chartered a Continuum of Care Advisory Team (CAT), to optimize the management and transition of patients across the care continuum and improve patient outcomes and experience. CAT members include representatives from ambulatory, hospital, and post-acute care physicians; business and strategic development; case management; health informatics; lean promotion office; nursing; organizational improvement; pharmacy; quality and safety; and rehab services. This multidisciplinary approach was used to overcome the barrier identified earlier of a lack of interdisciplinary transparency. The team operationalized the strategic plan by identifying strategies to align with the overall strategic plan, removing barriers, coordinating implementation, and spreading the improvements.
CAT established a continuum of care oversight structure focused on four objectives:
- Determine a single vision/goal and associated objectives, strategies, measures, and tactics for optimizing the continuum of care and reducing unwarranted variation.
- Coordinate, align, prioritize, package, commission, decommission, spread, and identify venues/tools to support the continuum of care for the health system.
- Accelerate and control the spread of continuum of care work to all appropriate areas of care.
- Evaluate and respond to key performance indicators.
Using lean methods, The University of Kansas Health System developed a standard process to prevent 30-day readmissions by uncovering and responding to the underlying causes for readmission. This was largely accomplished by focusing on the role that chronic disease progression played in readmissions, and differentiating among patients based on their underlying disease, comorbidities, and post-discharge care settings. Five activities aimed at reducing the 30-day readmission rates were subsequently implemented:
- Established the patient family advisory council to gain insight into contributing factors for readmission.
- Provided education on the implementation of counter measures designed to prevent readmission.
- Developed and implemented the hospital-to-home program for Medicare patients with the diagnosis of heart failure. The program included a follow-up call to the patient at 24 to 48 hours, seven to 10 days, and 30-days post discharge, as well as home visits to high-risk patients. The organization expanded the program to include all insured patients age 18 or older with more than one readmission the previous 30 days, who would now receive the increased follow-up protocol to bridge the patient with a primary care provider and other resources.
- Developed and implemented standard protocols for patients with comorbidities.
- Established a preferred network for skilled nursing, home health, and hospice placement.
Clinicians use the data within the advanced analytic application to identify patients at highest risk for readmission, and implement the appropriate countermeasures to prevent an avoidable, costly readmission.
RESULTS
Using machine learning, predictive analytics, and lean care redesign, The University of Kansas Health System accurately identified patients at highest risk of readmission and guided clinical interventions, which resulted in substantial reduction in 30-day readmission rates:
- 39 percent relative reduction in all-cause 30-day readmissions.
- 52 percent relative reduction in 30-day readmission of patients with a principle diagnosis of heart failure.
Additional readmission rate reductions were realized for those patients enrolled in the hospital-to-home program:
- 42 percent relative reduction in all-cause 30-day readmissions.
- 49 percent relative reduction in 30-day readmission of patients with a principle diagnosis of heart failure.
WHAT’S NEXT
Building on the success of this project, The University of Kansas Health System intends to continue using the same framework and methodology to drive improvements in other high-impact areas.
REFERENCES
- Hines, A. L., Barrett, M. L., Jiang, H. J., & Steiner, C. A. (2014). Conditions with the largest number of adult hospital readmissions by payer, 2011. Agency for Healthcare Research and Quality.
- Jencks, S. F., Williams, M. V., & Coleman, E. A. (2009). Rehospitalizations among patients in the Medicare fee-for-service program. The New England Journal of Medicine 360:1418-1428.
ABOUT HEALTH CATALYST
Health Catalyst is a next-generation data, analytics, and decision support company committed to being a catalyst for massive, sustained improvements in healthcare outcomes. We are the leaders in a new era of advanced predictive analytics for population health and value-based care. With a suite of machine learning-driven solutions, decades of outcomes-improvement expertise, and an unparalleled ability to integrate data from across the healthcare ecosystem. Our proven data warehousing and analytics platform helps improve quality, add efficiency and lower costs in support of more than 85 million patients and growing, ranging from the largest US health system to forward-thinking physician practices. Our technology and professional services can help you keep patients engaged and healthy in their homes and workplaces, and we can help you optimize care delivery to those patients when it becomes necessary. We are grateful to be recognized by Fortune, Gallup, Glassdoor, Modern Healthcare and a host of others as a Best Place to Work in technology and healthcare.
Visit www.healthcatalyst.com, and follow us on Twitter, LinkedIn, and Facebook.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.