Analytics Drive Lean Processes to Lower Healthcare-associated Infections

- Only one CAUTI in 1,861 days. Zero CAUTI in 747 days.
- Only one CLABSI in 824 days. Zero CLABSI in 332 days.
- 95th percentile patient satisfaction ranking.
Healthcare-associated infections (HAIs) remain one of the greatest risks patients face while hospitalized. Each day, about one in 25 hospital patients has at least one HAI—with an estimated 722,000 HAIs in U.S. acute care hospitals annually. Approximately 75,000 of the patients with HAIs died during their hospitalization.
The University of Kansas Health System, a large academic medical system with more than 80 locations across two states, experienced organizational central-line associated bloodstream infections (CLABSI) and catheter-associated urinary tract infection (CAUTI) rates that were higher than desired. A lack of consistent uniform evidence-based maintenance of indwelling urinary catheters and central lines led to unintended care variations, which is a challenge to large healthcare organizations.
Developing a reliable system for preventing CAUTI and CLABSI that produced consistent and accurate results would assist The University of Kansas Health System in HAI prevention. To create this solution, the health system chose to implement lean management for addressing both technical and adaptive work, applying data and analytics from its analytics platform to make improvements driven by lean methodologies.
HEALTHCARE-ASSOCIATED INFECTIONS UNDERMINE PATIENT SAFETY
Though largely preventable, HAIs continue to be a risk that patients face while hospitalized. Central-line associated bloodstream infections (CLABSI) and catheter-associated urinary tract infection (CAUTI) account for a significant portion of these infections.1 Each day, about one in 25 hospital patients has at least one HAI. It is estimated that 722,000 HAIs occur in U.S. acute care hospitals annually and approximately 75,000 patients with HAIs died during their hospitalization.2
Evidence-based intervention bundles could prevent CLABSI and CAUTI; however, translating them into practice requires an integrated approach that addresses both technical and adaptive work.3
One organization looking to address CLABSI and CAUTI rates was The University of Kansas Health System, a large academic medical system with more than 80 locations operating in two states, 999 licensed beds, over 700 employed physicians and 10,000 employees, which has a vision of leading the nation in caring, healing, teaching, and discovering. Recognizing HAIs’ risk to patient safety, the health system committed to reducing the occurrence of HAIs and striving for zero harm.
STANDARDIZING BEST PRACTICES
Any large healthcare organization experiences unintended care variations. Often, and as was the case with The University of Kansas Health System, the approach to best practice differs by patient population and care location. Methods for communicating and confirming changes in patient care needs also vary. While evidence-based criteria for insertion and maintenance of indwelling urinary catheters and central lines existed, the understanding and utilization of them varied between medical service, nursing units, and in some cases, even shift to shift.
Further complicating efforts to improve CAUTI and CLABSI rates was the lack of meaningful performance data. Nursing and medical staff were often unaware of the impact of the care they provided on CAUTI and CLABSI rates. Obtaining this information was burdensome, limiting the ability to link care delivered to specific outcomes.
For The University of Kansas Health System, organizational CAUTI and CLABSI rates were higher than desired. The organization needed to change its approach to preventing CAUTI and CLABSI and develop a reliable system that produced consistent, accurate results.
LEAN MANAGEMENT FOR HAI PREVENTION
To lower CAUTI and CLABSI rates, The University of Kansas Health System chose to implement lean management as a mechanism to address both technical and adaptive work. It also applied data and analytics from the Health Catalyst® Data Operating System (DOS™) Platform to make improvements driven by lean methodologies.
Training for consistency across care teams
The University of Kansas Health System prepares and engages organizational leaders in managing lean improvement work to systematically spread and govern standard efforts across various workgroups. Lean training is provided for a variety of levels, including courses for those who are new to lean improvement work, training for all health system employees, and hands-on development for frontline leaders.
To drive reductions in CAUTI and CLABSI rates, the medical progressive care unit used rapid improvement events to develop and implement standard work for CAUTI and CLABSI prevention. This includes maintenance bundles, compliance with evidence-based criteria for insertion of indwelling urinary catheters and central lines, and consistent utilization of a nurse-driven protocol for discontinuation of indwelling urinary catheters.
After deploying the standard work for CAUTI and CLABSI prevention, the unit within the health system trained all employees involved in CAUTI and CLABSI prevention, ensuring a shared understanding of organizational expectations for the care patients should receive. Nursing staff obtained education on the bundle elements demonstrated to prevent a CAUTI and CLABSI including, but not limited to the use of securement devices, emptying of indwelling urinary catheters at least every four hours, appropriate hygiene practices each shift, and appropriate line maintenance.
Integrating lean processes into daily routine
Once training is completed, this model cell unit ensures this focus and review of bundle elements are incorporated into the daily routine for each shift, in a proactive, rather than reactive approach. The medical progressive care unit uses its lean management system to ensure ongoing process improvement, application of the standard work, and consistent delivery of care throughout the day. Additionally, the nursing staff comes together at a unit level to huddle multiple times each day. These structured huddles ensure the nursing unit is ready for the day and has the correct methods, equipment, supplies, and staffing to meet patient needs and perform the required work.
The nursing staff’s structured huddles also provide an opportunity to escalate barriers impeding implementation of the standard work or best practice, including CAUTI and CLABSI prevention. For example, patients occasionally decline indwelling urinary catheter care. If the registered nurse (RN) providing care to the patient is unable to solicit the patient’s participation in catheter care, the RN can escalate the issue to the charge RN. Issues can be elevated to the nurse manager, infection preventionist, or physician as needed. The interdisciplinary teams collaborate with the consistent focus of prevention to an HAI and supporting optimal patient outcomes.
Analytics drive improved lean processes
The University of Kansas Health System integrates data from the analytics platform into its lean management system to further drive results. Information is available for the entire health system and can be filtered to the specific department, unit, provider, procedure, or patient of interest. Performance data is reviewed at all levels in an action-oriented process that has leaders and frontline staff actively identifying the barriers impeding performance, taking action to address the obstacles and improve performance.
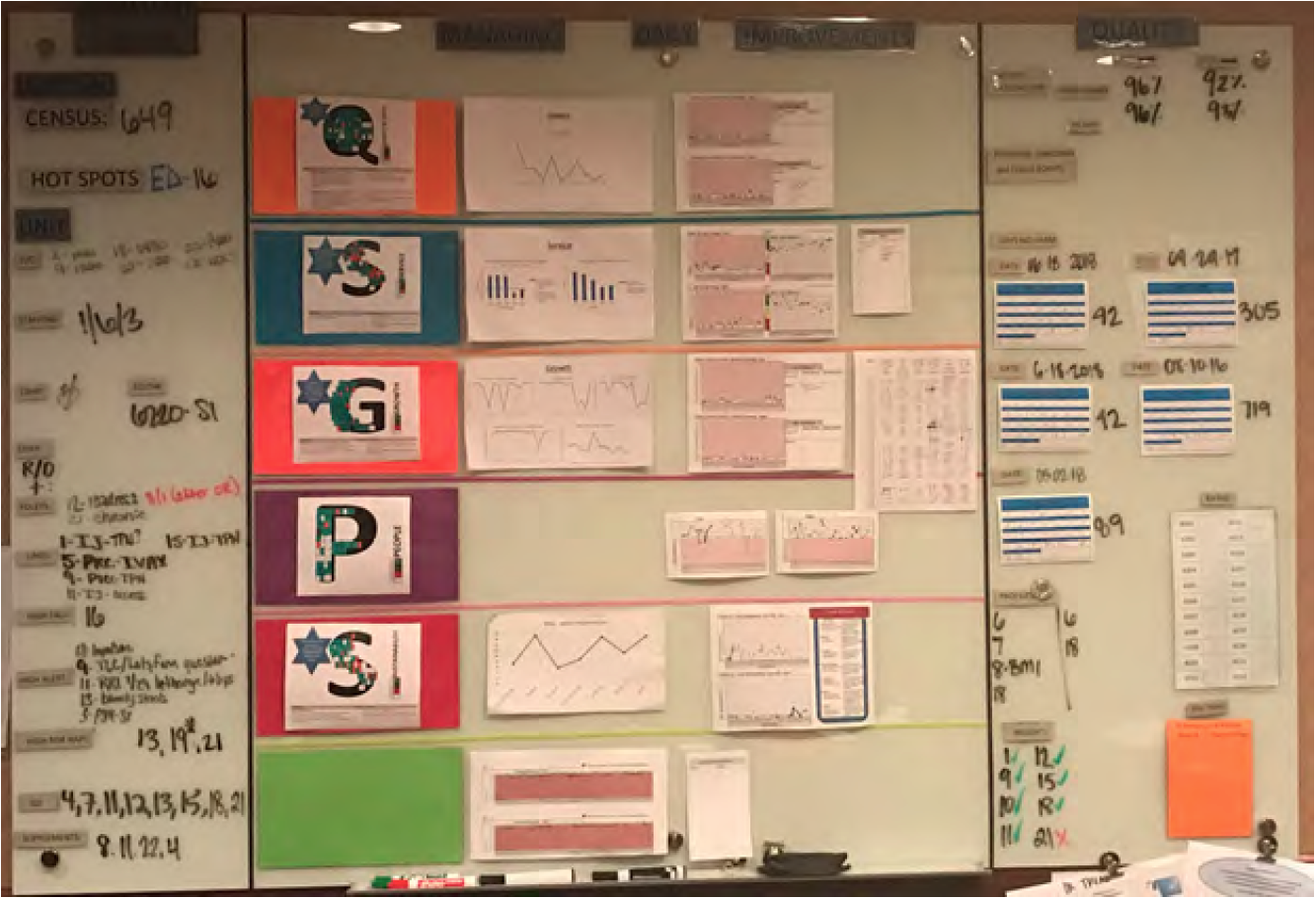
The nursing unit integrates data from the analytics platform into the visibility boards used during the huddles, providing frontline staff with their specific unit level performance data (see Figure 1). Each shift huddle utilizes the visibility board to review performance in five categories: quality and safety; service; growth; people; and sustainability. For the first time, frontline staff can visualize and understand the impact of their standard daily work on unit and organization-wide CLABSI and CAUTI rates as well as other metric goals.
The nursing unit has also created a sense of ownership and accountability for performance. The structured huddles, meaningful data that links specific actions to patient outcomes, and direct observation of performance, have fostered the development of a culture of ownership focused on quality outcomes. Frontline staff review their unit level CLABSI and CAUTI daily and can readily state the number of days since the last infection. Additionally, each day the team is able to share the current status of patients and plan in place to prevent a potential HAI.
RESULTS
The University of Kansas Health System’s lean management system, combined with meaningful data and analytics, has successfully reduced HAIs for patients admitted to the medical progressive care unit. Results include:
- Only one CAUTI in 1,861 days. Zero CAUTI in 747 days.
- Only one CLABSI in 824 days. Zero CLABSI in 332 days.
- 95th percentile patient satisfaction ranking.
“We lacked a data platform that would allow us to provide staff specific feedback about their performance. Data and performance were disassociated from the nursing staff’s workflow. Now, we have unit level performance data and can link our staff’s performance to the patient’s outcomes.”
– Tori Butler, MSN, RN, NEA-BC
Nurse Manager
WHAT’S NEXT
The University of Kansas Health System plans to continue applying data, analytics, and lean six sigma methodologies to drive improvement across the entire organization.
REFERENCES
- Agency for Healthcare Research and Quality. (2017). Health Care-Associated Infections.
- Centers for Disease Control and Prevention. (2018). HAI data and statistics.
- Septimus, E. J., & Moody, J. (2016). Prevention of device-related healthcare-associated infections. F1000Research, 5, F1000 Faculty Rev–65.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.