The Healthcare Analytics Adoption Model: A Roadmap to Analytic Maturity
The focus on analytics is contributing to the “EHR problem”—doctors prioritizing the EHR over patients. The Healthcare Analytics Adoption Model (HAAM) walks healthcare organizations through nine levels that lay the framework to fully leverage analytic capabilities to improve patient outcomes:
Level 1. Enterprise Data Operating System
Level 2. Standardized Vocabulary & Patient Registries
Level 3. Automated Internal Reporting
Level 4. Automated External Reporting
Level 5. Waste and Care Variability Reduction
Level 6. Population Health Management & Suggestive Analytics
Level 7. Clinical Risk Intervention & Predictive Analytics
Level 8. Personalized Medicine & Prescriptive Analytics
Level 9. Direct-To-Patient Analytics & Artificial Intelligence
Analytics are crucial to becoming a data-driven organization, but providers and administrators can’t forget about the why behind the data—to improve outcomes. Following the HAAM enables organizations to build a sustainable, analytic platform and empower patients to become data-driven when it comes to their own care.
This report is based on a 2020 webinar given by Dale Sanders, Chief Technology Officer, Health Catalyst, entitled, “Reviewing the Healthcare Analytics Adoption Model: A Roadmap and Recipe for Analytic Maturity”.
Across the country, health systems are losing providers due to burnout. As leaders in healthcare know, data and analytics can help the situation or exacerbate it. Although analytics play a critical role in healthcare improvement, in some cases the focus of data can actually contribute to burnout through the increasing “EHR problem”—prioritizing the EHR over patients.
Danielle Ofri, MD, at Bellevue Hospital poses a question to healthcare providers everywhere, “The aggressiveness of the EMR’s incursion into the doctor–patient relationship has forced us to declare our loyalties: are we taking care of patients or are we taking care of the EMR?”
Data Analytics Is Part of the Problem
The EHRs are taking the blame, but an over-focus on data is also part of the problem. The proliferation of all quality measures and reporting—and the burden that it places on physicians—is doing the opposite of what health systems are trying to achieve with data. Rather than simplifying processes and improving care, the focus on data can make care delivery unnecessarily complex, resulting in wasted resources as a health system tries to become data driven.
The Healthcare Analytics Adoption Model (HAAM) provides healthcare organizations with a framework to follow in order to fully leverage the capabilities of analytics and achieve the primary goals of using data in healthcare— to improve patient outcomes while cutting costs, decreasing provider burnout, and maintaining patient satisfaction.
Sanders’s Hierarchy of Analytics Needs 2002
In 2002, the HAAM framework (Figure 1), was Dale Sanders’s, now Chief Technology Officer at Health Catalyst, first model for guiding health systems through analytic maturity. At step one, health systems needed to focus on adhering to compliance and regulatory measures, then accreditation (e.g., Joint Commission). Then, systems could focus on accreditation and professional societies, (e.g., STS, etc.,) followed by meeting payer financial incentives. After that, the focus turned to implementing evidence-based medicine routinely practiced throughout the organization.
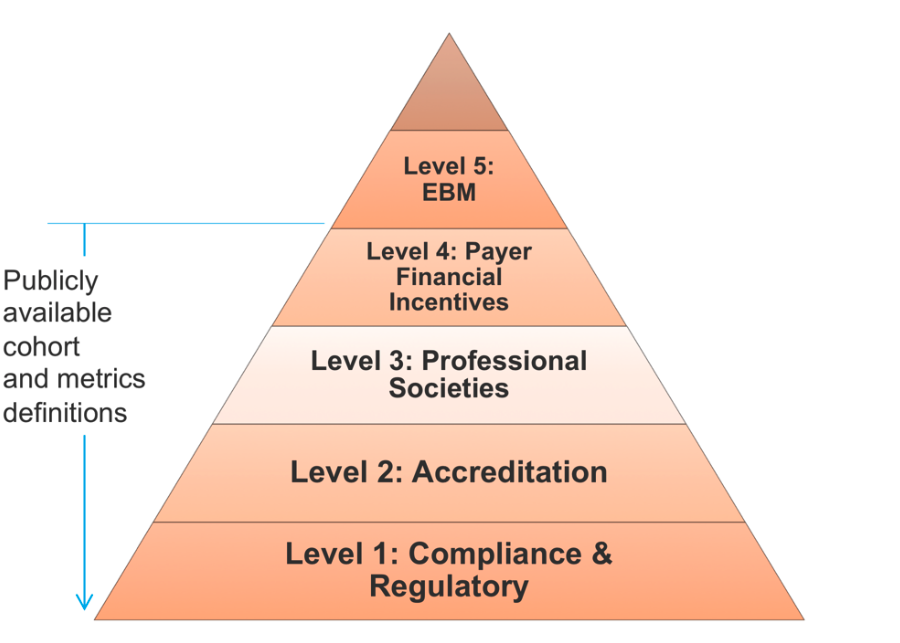
Figure 1. Hierarchy of Analytics Needs, 2002.
As a first attempt at creating an analytics adoption model, it captured the basics, but lacked definition and left room for growth as the industry expanded/evolved overtime.
Healthcare Analytics Adoption Model, 2013
By 2013, as health systems were maturing and leveraging analytics at a deeper level, the HAAM followed suit by adding three more levels that focused on automation, machine learning (ML), and a more individualized approach to medicine.
The model also matured to emphasize the basics for analytics acumen—levels three and four, the basic internal and external reporting requirements—before moving to levels five and above. The inefficiencies and overwhelming number of quality measures and KPIs in levels three and four were a roadblock for many health systems, so it was critical to increase the efficiency and the productivity at levels four and below in order to move forward.
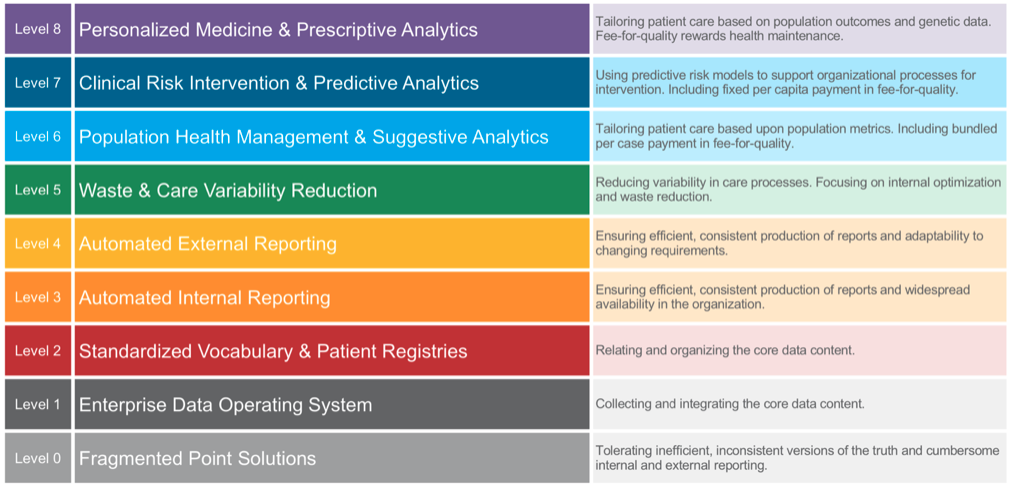
Figure 2. The Healthcare Analytics Adoption Model, 2013.
HIMSS and Health Catalyst Adoption Model for Analytic Maturity, 2015
In 2015, Health Catalyst and Healthcare Information and Management Systems Society (HIMSS) saw the need to create a standard model for analytic maturity, so they teamed up to create an official Adoption Model for Analytic Maturity (Figure 3) that could serve as the industry standard—disconnected from any vendor.
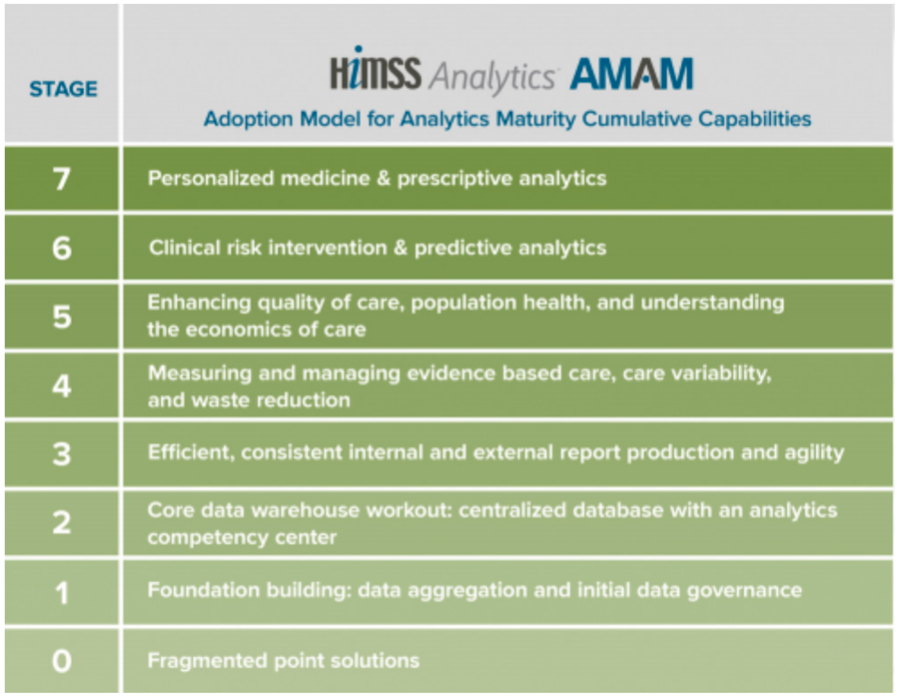
Figure 3. Adoption Model for Analytics Maturity. Source: HIMSS Continuity of Care Matrix.
HAAM 2019
The latest version of HAAM (Figure 4) is based largely on the original model. Currently, Dr. Anne Snowdon, Director of Clinical Research at HIMSS Analytics, and Dale Sanders are working together to ensure the modifications are collaborative and supportive of HIMSS’s initiatives, by adding Level 9—focused on increasing patients’ analytics acumen and helping them become data-driven when it comes to their own care.
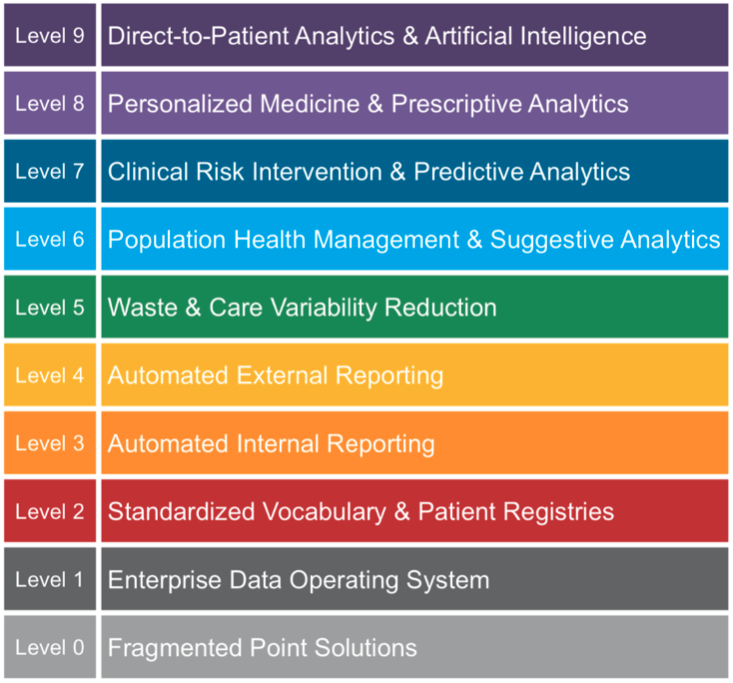
Figure 4. The Healthcare Analytics Adoption Model, 2019
The Healthcare Analytics Adoption Model at Every Level
Level 0. Fragmented Point Solutions
Vendor-based and internally developed applications are used to address specific analytic needs as they arise, but the fragmented point solutions are neither co-located in a data warehouse nor otherwise architecturally integrated with one another. Overlapping data content leads to multiple versions of analytic truth, making reporting labor-intensive and inconsistent. At this point, data governance is non-existent.
Level 1. Enterprise Data Operating System
At a minimum, the following data are co-located in a single data warehouse, locally or hosted: HIMSS EMR Stage 3 data, revenue cycle, financial, costing, supply chain, and patient experience. A searchable metadata repository is available across the enterprise. Data content includes insurance claims, if possible. The data warehouse is updated within one month of source system changes and data governance is forming around the data quality of source systems. The enterprise data warehouse reports organizationally to the chief information officer.
Level 2. Standardized Vocabulary and Patient Registries
Master vocabulary and reference data are identified and standardized across disparate source system content in the data warehouse. Naming, definition, and data types are consistent with local standards and patient registries are defined solely on ICD billing data. Data governance forms around the definition and evolution of patient registries and master data management.
Level 3. Automated Internal Reporting
Analytic motive is focused on consistent, efficient production of reports that support basic management and operation of the healthcare organization. Key performance indicators are easily accessible from the executive level to the front-line manager. Corporate and business unit data analysts meet regularly to collaborate and steer the EDW. Data governance expands to raise the data literacy of the organization and develop a data acquisition strategy for Levels 4 and above.
Level 4. Automated External Reporting
The analytic motive is focused on consistent, efficient production of reports required for regulatory and accreditation requirements (e.g., CMS, Joint Commission, tumor registry, communicable diseases); payer incentives (e.g., MU, PQRS, VBP, readmission reduction); and specialty society databases (e.g., STS, NRMI, Vermont-Oxford). Adherence to industry-standard vocabularies is required at this point. Clinical text data content is available for simple keyword searches and centralized data governance exists for review and approval of externally released data.
Level 5. Waste and Care Variability Reduction
Analytic motive is focused on measuring adherence to clinical best practices, minimizing waste, and reducing variability. At this point, data governance expands to support care management teams that are focused on improving the health of patient populations, population-based analytics are used to suggest improvements to individual patient care and permanent multidisciplinary teams are in-place that continuously monitor opportunities to improve quality and reduce risk and cost, across acute care processes, chronic diseases, patient safety scenarios, and internal workflows. Precision of registries is improved by including data from lab, pharmacy, and clinical observations in the definition of the patient cohorts. EDW content is organized into evidence-based, standardized data marts that combine clinical and cost data associated with patient registries. Data content expands to include insurance claims (if not already included) and HIE data feeds and the EDW is updated within one week of source system changes.
Level 6. Population Health Management and Suggestive Analytics
The “accountable care organization” shares in the financial risk and reward that is tied to clinical outcomes. At least 50% of acute care cases are managed under bundled payments. Analytics are available at the point of care to support the Triple Aim of maximizing the quality of individual patient care, population management, and the economics of care. Data content expands to include bedside devices, home monitoring data, external pharmacy data, and detailed activity-based costing. Data governance plays a major role in the accuracy of metrics supporting quality-based compensation plans for clinicians and executives. On average, the EDW is updated within one day of source system changes. The EDW reports organizationally to a C-level executive who is accountable for balancing cost of care and quality of care.
Level 7. Clinical Risk Intervention and Predictive Analytics
Analytic motive expands to address diagnosis-based, fixed-fee per capita reimbursement models. Focus expands from management of cases to collaboration with clinician and payer partners to manage episodes of care, using predictive modeling, forecasting, and risk stratification to support outreach, triage, escalation, and referrals. Physicians, hospitals, employers, payers, and members/patients collaborate to share risk and reward (e.g., financial reward to patients for healthy behavior). Patients are flagged in registries who are unable or unwilling to participate in care protocols. Data content expands to include home monitoring data, long term care facility data, and protocol-specific patient-reported outcomes. On average, the EDW is updated within one hour or less of source system changes.
Level 8. Personalized Medicine & Prescriptive Analytics
Analytic motive expands to wellness management, physical and behavioral functional health, and mass customization of care. Analytics expands to include NLP of text, prescriptive analytics, and interventional decision support. Prescriptive analytics are available at the point of care to improve patient-specific outcomes based upon population outcomes. Data content expands to include 7×24 biometrics data, genomic data, and familial data. The EDW is updated within a few minutes of changes in the source systems.
Level 9. Direct-To-Patient Analytics & Artificial Intelligence
Analytics and artificial intelligence (AI) are provided directly to patients, which enables greater personal ownership and precision in their health decisions. With more knowledge and involvement in their care, patients become data-driven, along with their healthcare team.
Direct-to-patient analytics and AI are used in a collaborative decision-making environment between patients and healthcare providers. Patients have the ability to port and analyze their complete healthcare data ecosystem, independent of healthcare providers. Treatment and health maintenance protocols are enabled using AI-based digital twins– “Patients Like This” and “Patients Like Me” pattern recognition.
The Healthcare Analytics Adoption Model: Key to Analytic Maturity
Health systems know that accurate data is essential to become a data-driven organization, but the only way to achieve sustainable and effective analytics adoption is to follow a proven framework. The HAAM is specifically designed—over multiple iterations since 2002—for healthcare organizations and the unique challenges they face when it comes to data.
Following the HAAM, healthcare organizations can build a sustainable, analytic platform to leverage analytic–a must-do in order to survive as reimbursements and measures shift the focus from volume to value. With a strong analytic framework, health systems can leverage data to drive outcomes improvement and stay focused on patients instead of the EHR.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.
