Trigger-Based Analytics Application Recognizes More Wrong-Patient Order Errors

- For the first time, the organization has comprehensive wrong-patient order data, and has the ability to truly understand the number of wrong-patient orders.
This healthcare organization, comprised of a specialty hospital and multiple clinics, sought to improve safety for its patients, focusing on identifying wrong-patient order errors. To better understand and improve patient safety, the organization needed to move beyond passive surveillance. By using multiple detection methods for identifying wrong-patient errors and establishing triggers that identify when a wrong-patient order may have occurred, hospital and clinic staff are able to investigate instances.
WRONG-PATIENT ERRORS: A SIGNIFICANT PATIENT SAFETY RISK
There are more than 600,000 wrong-patient orders each year in the U.S.1 Despite a lack of evidence about the root cause of these errors, many experts believe that wrong-patient errors increase when clinicians have more than one electronic chart open.2 Numerous studies have demonstrated the benefit of triggers to identify potential adverse events.3 Retract-and-reorder triggers, which identify when an order has been placed for a patient, retracted, and re-ordered by the same clinician, have demonstrated effectiveness in identifying the incidence of wrong-patient orders, but few healthcare organizations have implemented and operationalized triggers to identify wrong-patient errors and improve patient safety.3,4
PASSIVE SURVEILLANCE DOES NOT IDENTIFY WRONG-PATIENT ORDERS
The organization had a well-established passive surveillance strategy in place for voluntary reporting of errors and near misses. However, it recognized that passive surveillance has its limitations and likely underrepresented the number of wrong-patient order errors, as the errors were rarely reported through its voluntary reporting process.
To better understand and improve patient safety, the organization needed to move beyond passive surveillance, using multiple detection methods for identifying errors occurring in the ordering process. It had attempted to use triggers to understand wrong-patient order errors previously, but the process was so laborious, it limited the ability of the organization to use triggers to understand performance and improve patient safety.
Because of the time required for manual review, any available data was of limited use. The organization needed to automate the recognition of wrong-patient orders, as well as the identification of the factors contributing to the error so that it could implement system-based risk reduction strategies to prevent similar errors in the future.
ACTIVE TRIGGERS WARN OF WRONG-PATIENT ORDERS
To truly understand prescribing safety, the organization leveraged the Health Catalyst® Data Operating System (DOS™) and a robust suite of analytics applications, including the Patient Safety Monitor™ Suite: Surveillance Module, a trigger-based surveillance system, to monitor, detect, predict, and prevent threats to patient safety before harm can occur.
The organization implemented a trigger to identify wrong-patient orders. The “wrong patient retract and reorder” trigger uses information from the data platform to detect any incorrect patient orders, including medication, imaging, and labs. The analytics application uses data to identify when a clinician incorrectly places an order, such as in situations where a clinician places an order for patient A, discontinues that order, then reorders the same thing for patient B within a short timeframe.
When this error type is recognized, the trigger fires and is presented in the analytics application. The visualization in the analytics application includes detail about the triggering event, including the order name, cancellation date/time, order date/time, and the ordering provider (see Figure 1).
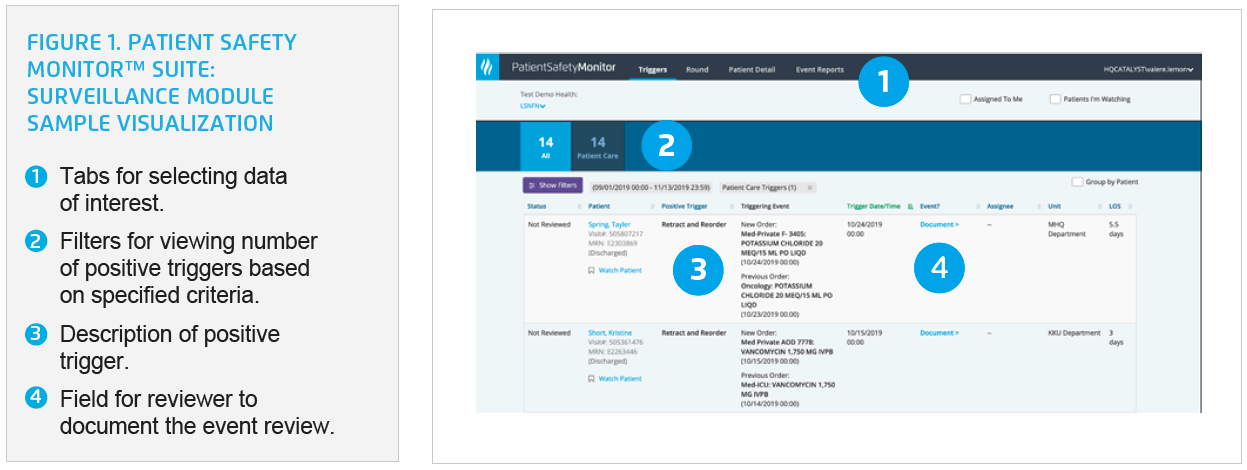
Trained staff is then tasked with reviewing the trigger from the initial fire. Reviewers use the chart review function in the analytics application to access patient-specific data and the case details. They then evaluate the wrong-patient order error to verify if the order was placed for the wrong patient. If there was an error, reviewers inquire about the reason for the error and document what’s reported.
The organization established guidelines outlining the timeframes for investigating and communicating wrong-patient order errors, as well as guidelines for which events are appropriate for entry into the electronic error reporting system. Data are collected and analyzed to examine the factors contributing to the error and demographics, such as clinician, location, and order. The organization also documents selected near-miss wrong-patient order events in the electronic error reporting system. This information is used to identify improvement strategies. Triggers provide a consistent means of data collection, allowing the organization to monitor trends over time.
RESULTS
For the first time, the organization has comprehensive wrong-patient order data and can truly understand the number of wrong-patient orders occurring. It can visualize the rate of wrong-patient orders on a control chart and can visualize variation over time, enabling staff to evaluate the impact of process changes on safety.
The triggers-based analytics application identified more wrong-patient orders than reported as part of the voluntary reporting system. The analytics application has also dramatically reduced the time required to review safety events.
The triggers-based analytics application has allowed the organization to identify several factors contributing to the wrong-patient order errors, informing improvement plans to mediate the risk for harm. These errors include:
- Clicking the wrong-patient medical record number in the EMR.
- Interruptions during the order entry process.
- Similarly named patients.
The organization can now learn from its wrong-patient order trigger data, and leadership can begin to understand what a “good” rate is for the number of errors. Going forward, it will integrate the trigger data into ongoing operations to monitor and improve performance.“The best way to learn why prescribing errors occur, is to see what near-miss events are happening. Once you understand the root cause, you can implement system changes to prevent patient harm.”
– Pharmacist
WHAT’S NEXT
The organization continues to refine the triggers across a range of areas that indicate potential error or harm, including use of predictive models and AI, and is continuing to add additional triggers to improve event detection, further accelerating its efforts to build a culture of safety that is focused on achieving zero harm.
REFERENCES
- Columbia University Irving Medical Center. (2019). Do electronic health records cause patient mixups?
- Adelman, J. S., Applebaum, J. R., Schechter, C. B., Berger, M. A., Reissman, S. H., Thota, R., Racine, A. D., Vawdrey, D. K., Green, R. A., Salmasian, H., Schiff, G. D., Wright, A., Landman, A., Bates, D. W., Koppel, R., Galanter, W. L., Lambert, B. L., Paparella, S., & Southern, W. N. (2019). Effect of Restriction of the Number of Concurrently Open Records in an Electronic Health Record on Wrong-Patient Order Errors: A Randomized Clinical Trial. JAMA, 321(18):1780–1787.
- Dean Sittig, D. & Singh, H. (2015). The health IT safety center roadmap: What’s next? Health Affairs Blog.
- Adelman, J. S., Kalkut, G. E., Schechter, C. B., Weiss, J. M., Berger, M. A., Reissman, S. H., Cohen, H. W., Lorenzen, S. J., Burack, D. A., & Southern, W. N. (2012). Understanding and preventing wrong-patient electronic orders: a randomized controlled trial. J Am Med Inform Assoc., 20(2):305-10
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.