Readiness Assessment Key to Sustainable Outcomes Improvement

- Competency for improving outcomes measured at the organization, department, and role level.
- Recommendations made for increasing competency levels across the organization.
- Clear direction and focus obtained from opportunity analysis.
Experiencing pockets of success is not enough to prosper during the transformation to value-based care. Leaders at UnityPoint Health, a healthcare system serving Iowa, western Illinois, and southern Wisconsin, determined that outcomes improvements needed to be sustained and spread easily across the organization to best utilize resources and serve its patients.
UnityPoint Health required an objective way to understand the strengths and weaknesses of the organization relative to outcomes improvement and its readiness for change. To this end, it chose the Health Catalyst® Outcomes Improvement Readiness Assessment (OIRA) Tool and professional services to administer it and identify the competency levels in the organization in the five areas known to influence an organization’s readiness for change.
UNDERSTANDING ORGANIZATIONAL READINESS
Healthcare is undergoing a significant transformation requiring better patient outcomes at a lower cost.1 Experiencing pockets of success is not enough to survive and thrive through that transformation. Underlying the successful implementation of new policies, programs, and practices in healthcare settings is the organizational readiness and willingness to accept change. Understanding their own organizational readiness will assist healthcare leaders in reducing the number of change efforts that do not achieve the desired benefits.2
UnityPoint Health is the nation’s 13th largest nonprofit health system and the fourth largest nondenominational health system in America. As a network of hospitals, clinics, and home care services, it provides care throughout Iowa, western Illinois, and southern Wisconsin. Because it is such a large system operating across three states, the ability to transfer best practices from one site to another is particularly important to the organization.
Leadership at UnityPoint Health determined that outcomes improvements that cannot be sustained and spread easily across locations are a waste of resources and ultimately do not serve its patients. They were starting a new chapter in improving clinical outcomes and in search of a methodology for outcomes improvement that could be easily prioritized, supported and resourced, replicated and sustained across the organization, and that would consistently deliver the desired benefits.
GAINING DEEPER ORGANIZATIONAL KNOWLEDGE
UnityPoint Health recognized that without understanding its strengths and weaknesses regarding readiness for change, it would consistently run into the same barriers to achieving its vision of sustainable outcomes improvement.
Five organizational aspects influence the ability to improve the spread and adoption of outcomes improvement:
- The right leadership, culture, and governance in place to embrace change.
- The infrastructure and data sources to support effective and accurate analytics.
- The infrastructure and buy-in to promote best practice.
- The right team structure and champions to foster adoption.
- The correct payment structure and financial alignment to provide the funds to support appropriate patient care.
The first challenge for UnityPoint Health was to identify the organizational competencies that contribute to success in each of those five categories and then to evaluate the level of those competencies within UnityPoint Health. The next step was to identify and prioritize improvement opportunities and ensure that the organization had the necessary competency level in the five areas to obtain and sustain the desired outcomes.
IDENTIFYING AND MEASURING ORGANIZATIONAL COMPETENCY
Looking for an objective way to understand the strengths and weaknesses of the organization and its readiness for change, UnityPoint Health decided to use the OIRA Tool and professional services of Health Catalyst to identify the organization’s competency levels in the five areas known to influence an organization’s readiness for change and success in outcomes improvement.
UnityPoint Health saw the OIRA Tool as an objective methodology to uncover a path forward to be most successful in reducing variation and adopting best practice across the organization. Its leadership knew that for the OIRA Tool to yield the most useful information, participants must be open and transparent about the current state of the organization and be willing to share the vision for the future. They also knew that they had to be willing to “go slow to go fast”—putting the time into thoughtful planning to avoid the costly time sink of unsuccessful or unsustained improvement efforts. Once the project was launched, it was necessary to monitor all concurrent projects to avoid over-committing resources, which can lead to the eventual failure of all projects being undertaken.
To practice these principles, UnityPoint Health leadership took the time to identify the key stakeholders and engaged their interest and enthusiasm to ensure the success and accuracy of the readiness assessment.
OUTCOMES IMPROVEMENT READINESS ASSESSMENT METHODOLOGY
The readiness assessment was conducted using on-site interviews conducted by Health Catalyst’s Professional Services. The data collected was analyzed and placed into categories. For example, organizational strengths were identified during the onsite readiness assessment interviews by looking at the responses to the questions: “How would you describe your current leadership support?” and “What are the strengths of the organization?”
Potential risks were gleaned from the answers to “What are the opportunities (barriers) of the organization?” and other comments provided during the interviews.
The interviews were designed to identify the level of competency along 22 dimensions, which were organized into the five categories known to influence an organization’s readiness for change. The resulting information was presented in spiderweb diagrams by organization, site, department, and role. A comparison of performance in each of the five areas was also compared to benchmarks to provide perspective. The highest and lowest competencies were highlighted and provided to leadership with the rest of the report (see Figure 1).
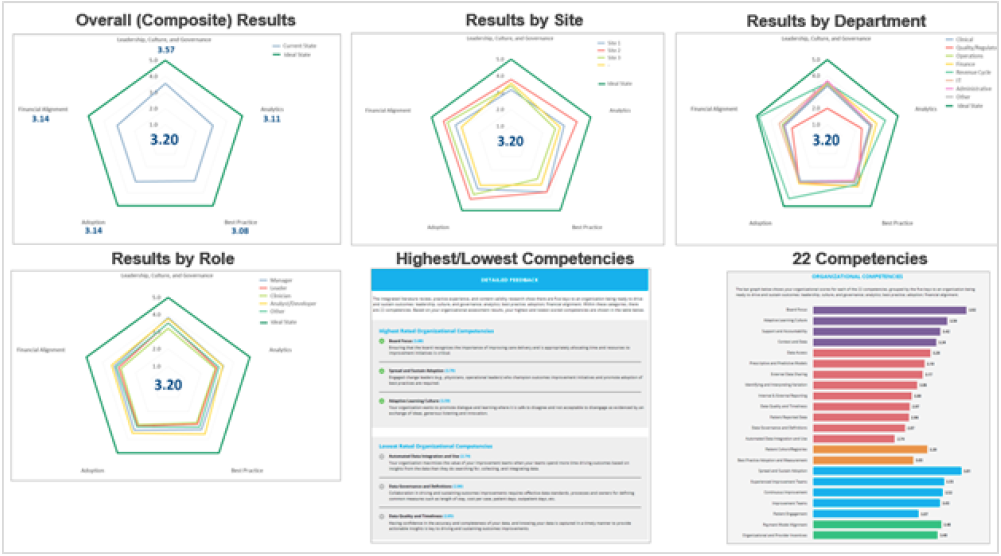
While the information and the recommendations obtained from the readiness assessment were not completely new to UnityPoint Health, it offered a perspective across the entire organization and interrelationships among the multiple sites which had previously been missing. So, while the insights were familiar, there was an element of surprise when the connections were seen.
OPPORTUNITY ANALYSIS METHODOLOGY
UnityPoint Health leadership also decided to use the Key Performance Analysis (KPA) application to produce an opportunity analysis that could be used in conjunction with the readiness assessment to optimize the focus of its improvement efforts fully.
The opportunity analysis was seen as a means to get the most out of limited resources by showing the organization which projects would produce the highest level of benefit to patients and the bottom line. By estimating the potential cost savings in each domain selected, it helped limit an over-commitment to too many unrelated and simultaneous projects, while still meeting organizational performance goals.
The first step of conducting a thorough opportunity analysis is data research, discovery, and gathering (see Figure 2). The main data sources used by UnityPoint Health were publicly available, client provided, and UnityPoint Health-specific information from the KPA application.
KPA predictions depend on calculations of potential volume and savings based on historical data specific to UnityPoint Health. The potential cost savings were based on current variation at a high level and calculated as result of achieving the mean. Continued refinement and new data will improve the accuracy of the cost savings predictions over time. This information was calculated by hospital, as well as rolled up to regions to provide the most insight.
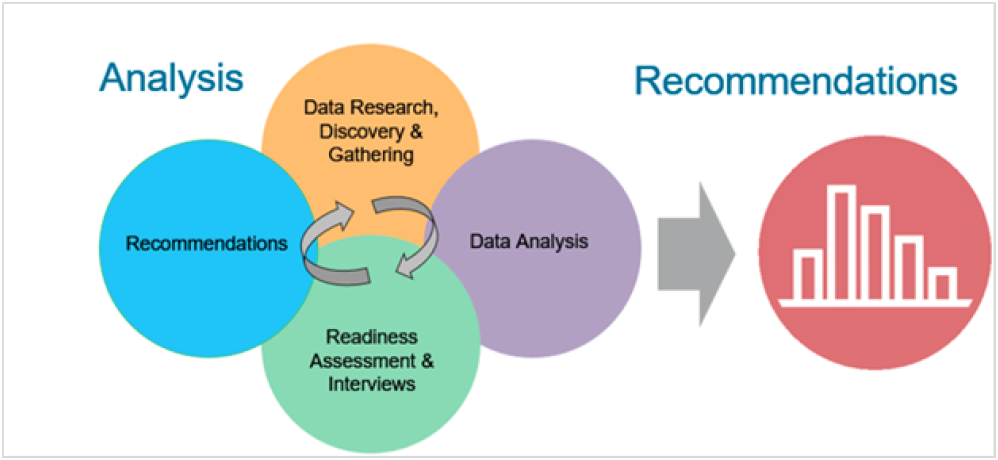
Once the data were gathered from these multiple sources, it was correlated, categorized, and analyzed to provide meaningful insight. Throughout this step, commonalities, consistencies, and variations were identified and examined for patterns and meaning.
Common alignments were identified as a result of the synthesis of the many different data sources used for the opportunity analysis. The commonalities from each of the sources were noted and specifically called out. The theory behind this approach is that if a weakness or problem area is cited in multiple sources, it is highly probable the potential opportunity is real and therefore should be labeled as a focus area. Common alignments and targeted themes were used to provide further depth to the opportunity analysis.
RESULTS
- Competency for improving outcomes measured at the organization, department, and role level.
- The readiness assessment yielded an analysis of competency at multiple levels of the organization. UnityPoint Health incorporated this knowledge into its decision-making and prioritization methodology to help it avoid barriers to achieving successful and sustained outcomes improvement.
- Recommendations made for increasing competency levels across the organization.
- Detailed recommendations for improving organizational competency in each of the five areas, (leadership, culture, and governance; analytics; best practice; and adoption), was provided to leadership and a plan for addressing each recommendation was quickly developed and implemented.
- Clear direction and focus obtained from opportunity analysis.
- Using data and analytics to develop a detailed opportunity analysis allowed UnityPoint Health to zero in on improvement initiatives that would be most beneficial to the patients and the organization. Coupling that information with its readiness assessment allowed the leadership team to prioritize and select a group of projects for which it had the necessary resources, capacity, and the organizational competency to accomplish.
“The readiness assessment allows us to focus and drive results quickly and sustainably. We are now able to match the qualitative readiness with the quantitative opportunity in an objective manner to understand the implications.”
– Rhiannon Harms, Executive Director, Analytics
WHAT’S NEXT
Armed with an objective understanding of its organizational strengths and weaknesses related to adopting and executing outcomes improvement, UnityPoint Health plans to use this information in conjunction with the opportunity analysis to develop a highly effective, data-driven methodology for consistently prioritizing, supporting, and sustaining outcomes improvement across the organization.
REFERENCES
- Becker’s Hospital Review. (2016). What clinical variation means to a hospital’s bottom line: 4 insights from the C-suite.
- Shea, C. M., Jacobs, S. R., Esserman, D. A., Bruce, K., & Weiner, B. J. (2014). Organizational readiness for implementing change: a psychometric assessment of a new measure. Implementation Science, 9(1), 7.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.