Data-Driven Operations Leverage Timely Data to Triple the Number of First Cases Starting on Time

- Tripled the number of first cases starting on time.
- Substantially reduced patient wait times, improving the patient experience.
- Additional insight into performance has helped create a culture where leaders and staff are using data to identify and implement continuous improvement.
Operating room (OR) costs are on the rise, with a single minute in the OR costing a hospital between $22 and $133 per minute. Providing patients with timely care is of the utmost importance, as even a slight delay in start time can cost healthcare organizations hundreds of thousands, if not millions, in lost revenue annually.
John Muir Health looked to reduce wasted time in the OR, focusing on first case on-time starts (FCOTS) as an important metric for improvement. However, OR teams were largely unaware of the importance of FCOTS, let alone how to improve the rates. In the OR, it was not uncommon for data to be three to six months old before being available for review, limiting the ability to use the data for improvement. As it was common for only 10 to 20 percent of cases to start on time in its OR, John Muir Health focused on providing the data needed to educate staff on the reasons behind delays, so that start times could be improved.
FIRST CASE ON-TIME STARTS: AN IMPORTANT MEASURE OF OPERATING ROOM EFFICIENCY
ORs are a critical source of patient care services and income generation for hospitals. However, ORs are also a source of high costs, with a single minute in the OR costing a hospital between $22 and $133 per minute.1,2 As a result, even a slight delay in start time can cost organizations hundreds of thousands, if not millions, of dollars annually.
First case on-time starts (FCOTS) are an important OR metric, providing insight on how timely and efficient care processes may be. First case delays create a ripple effect on OR operations for the remainder of the day, delaying subsequent cases, frustrating patients, decreasing efficiency, and increasing costs.3
A leader in healthcare in the San Francisco Bay Area, John Muir Health is a not-for-profit integrated system of doctors, hospitals, and other services. John Muir Health looked to reduce first case delays and improve its FCOTS as a means to improve OR efficiency and reduce unnecessary costs.
LACK OF PERFORMANCE DATA HINDERS IMPROVEMENT EFFORTS
John Muir Health’s surgical teams knew they needed to be more efficient to better meet patient care demands, but teams lacked the data to help them understand their performance. Operations in the OR were not data-driven, and it was not uncommon for data to be two to three months old before being available for review, limiting the ability to use the data for improvement efforts.
Surgical teams were largely unaware of the economic drivers within the OR, meaning staff was not fully aware of the importance of maintaining a high rate of FCOTS. While teams had started to discuss key performance indicators (KPIs), it had not been a priority. As a result, it was common for only 10 to 20 percent of cases in the OR to start on time.
Leadership at John Muir Health identified the need to improve OR efficiency. But before they would be able to do so, the teams needed actionable, timely data that could be used to inform improvement efforts.
REDUCING DELAYS WITH THE HELP OF DATA
To transform into a data-driven operation, John Muir Health leveraged the Health Catalyst® Analytics Platform and broad suite of analytics applications, specifically the Department Explorer: Surgical Services analytics application, to better understand and improve operational efficiency within the OR.
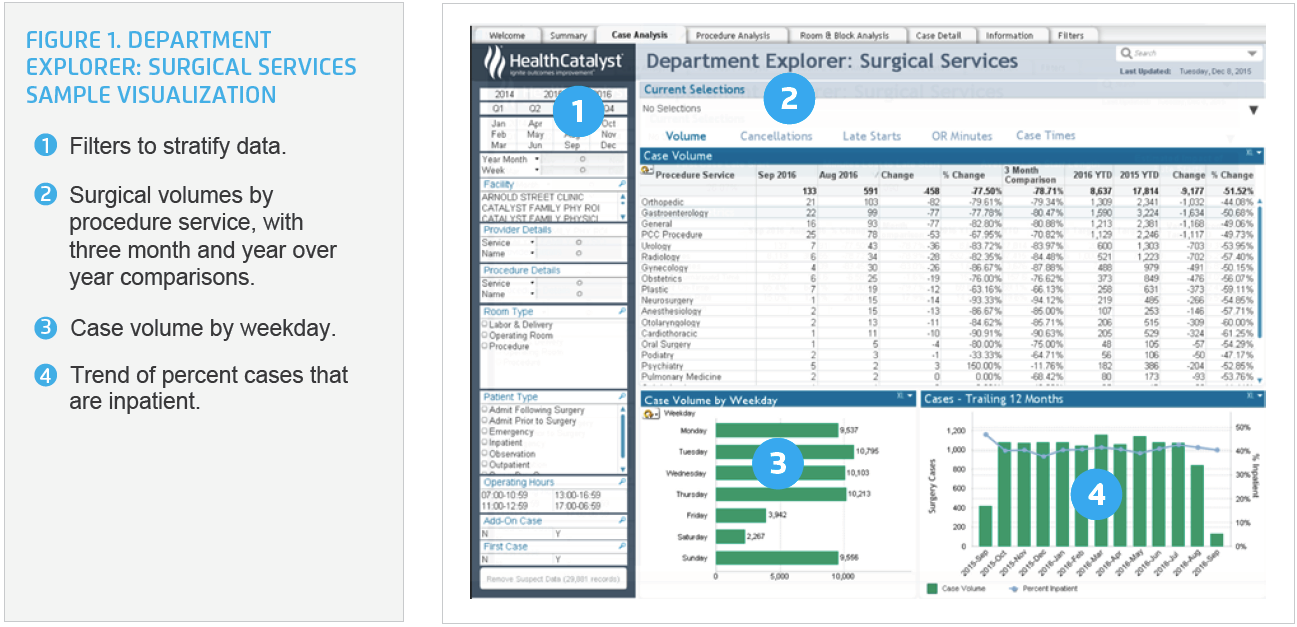
Department Explorer: Surgical Services is an analytics tool that provides managers multiple views of data regarding operational efficiency utilization, and case-level details specific to the OR (see Figure 1). This information helps users to better analyze specific OR data, such as patient prep, anesthesia prep, room turn-around, room and staff scheduling, and procedure data so that potential improvements can be identified.
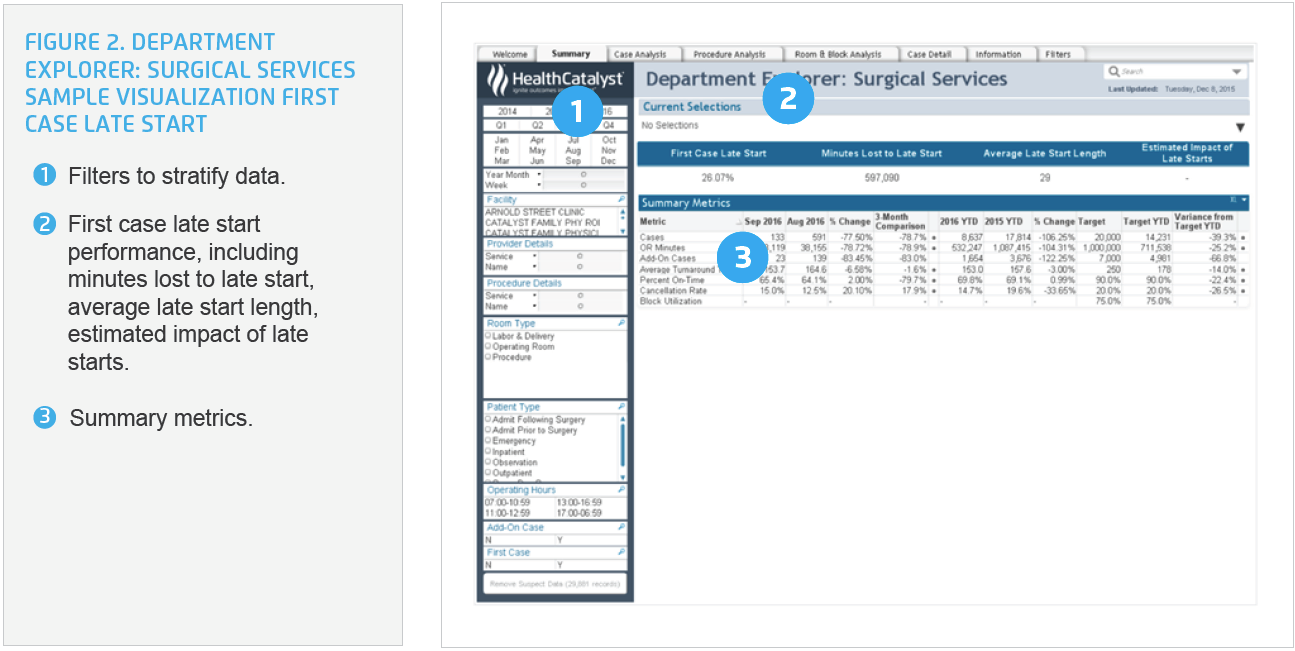
Using the analytics application, surgical services leadership was able to drill into OR KPIs, including FCOTS (see Figure 2). For the first time, leadership was able to slice and dice the data to understand the reasons for delays. Leaders were able to easily identify outliers, and opportunities for improvement.
With improved access to actionable data, surgical services leadership began engaging nursing staff and surgeons to understand their performance data and use it for improvement. First, leaders socialized the data with the team, reviewing and validating that data were correct. During this process, they identified an opportunity to improve delay codes, ensuring hospital staff was using a small list of delay codes that were meaningful.
Leaders implemented processes to ensure timely, actionable data was shared with nursing staff and surgeons on a regular basis. The medical director engaged his colleagues in peer-to-peer conversations about performance, identifying opportunities for improvement and garnering their support to participate in improvement initiatives. The executive director for surgical services and other nursing leaders engaged their staff in similar conversations, providing them with the opportunity to question the data and give feedback based on their experience.
Improving FCOTS required a large number of key stakeholders perform work in concert with one another, coordinating complex care activities over a short period of time with the goal of the patient arriving in the OR as scheduled. This meant surgical teams, the patient, and the room and surgical equipment are all available and ready on time. Because such a large number of people are involved in care, leadership needed to meet with and engage a large number of stakeholders to implement changes, and then follow up with data to demonstrate the impact those changes had on performance.
Leaders regularly meet with various physician offices, engaging surgeons, directors, and office managers in improvement efforts, using data from the analytics platform to provide feedback about performance. The team used a data-driven approach to identify several process changes that improved the ability to start the first cases on time.
Pre-op changes
The pre-op team took greater responsibility for ensuring patients from the ICU arrived on time, taking ownership of the first case ICU transport. Pre-op nursing staff also took on greater responsibility for breathing treatments, ensuring patients receive needed treatments in a timely manner.
The data indicated that one factor contributing to late starts was patients who also required chemotherapy. Pharmacy staff would bring the chemotherapy medications to pre-op around 7:45 a.m., inadvertently contributing to delays. Leaders were able to provide the pharmacy team with this data, sharing the importance of the FCOTS as a KPI and as an economic driver. The pharmacy subsequently adjusted staff arrival time, bringing the chemotherapy medications to the OR earlier in the morning, helping to ensure on-time first case starts.
First case nerve blocks were also a source of delays. The teams now huddle each day, identifying how many first case nerve blocks are scheduled for the next day, adjusting staffing as needed to ensure adequate staff and an on-time start. Lastly, when patients arrived in the cold OR, they would indicate they needed to use the restroom. Pre-op nursing staff now take all patients who are able to use the restroom 30 minutes prior to the case start time.
Changes in OR procedures
The data indicated that delays in room set up, particularly for large cases, were negatively impacting the ability to start on time. To prevent this delay, the night shift charge nurse now works with staff to set up rooms more completely, preventing a delay in the morning.
When discussing opportunities for improvement, some staff shared that when they had large cases, they were arriving early to set up. Leadership invited all staff to have more control over their work, indicating that they were supportive of staff with large cases arriving early and clocking in, so they can be appropriately compensated for their work.
Changes in how performance is communicated to providers
After sharing the FCOTS data with providers and allowing adequate time for teams to adjust to new expectations for an on-time start, leadership began communicating surgeon specific performance through letters directly to surgeons. Over time, the individual letters changed to departmental letters. All department members are now able to see their performance in relation to their peers.
The team convenes for a huddle each afternoon, using data from the analytics application to review daily performance. They review the reason for any delays, actively engaging in identifying and implementing changes to prevent similar delays in the future.
RESULTS
John Muir Health is transforming into a data-driven OR, and its efforts to improve FCOTS is yielding the desired results. FCOTS data has been incorporated into daily workflows, supporting ongoing, active management of the start times. To date, and as a result of this improvement work, John Muir Health has successfully:
- Tripled the number of first cases starting on-time.
- Reduced the amount of time patients spend waiting for surgery, improving the patient experience.
While initially focused on improving FCOTS metrics, timely actionable data has resulted in:
- Additional insight into performance which has helped create a culture where leaders and staff are using data to identify and implement continuous improvement.
- For example, leaders identified the opportunity to improve how cases are scheduled and improve the block time assigned to each case.
“To improve operations, you need performance data that is immediately available, so that you can provide people with immediate feedback. Department Explorer: Surgical Services allows us to monitor our performance and provide immediate feedback to our teams.”
– Ryan B. Green, M.D., Ph.D.
Medical Anesthesia Consultants
WHAT’S NEXT
John Muir Health plans to continue to use a data-driven approach to improve performance. The health system’s leadership is continuing to work on decreasing waste, making processes less burdensome, and increasing OR efficiency.
REFERENCES
- Shippert, R. D. (2005). A study of time-dependent operating room fees and how to save $100,000 by using time-saving products. The American Journal of Cosmetic Surgery, 22(1), 25–34.
- Moore, M., Mallow, P. J., & Rizzo, J. A. (2014). The variable cost of an operating room minute for valvular procedures. Value in Health, 17(3):A112.
- Cox-Bauer, C. M., Greer, D. M., Vander-Wyst, K. B., & Kamelle, S. A. (2016). First-case operating room delays: Patterns across urban hospitals within a single health care system. Journal of Patient-Centered Research and Reviews, 3(3):125-35
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.